Abstract
Background and Aims: Splanchnic vein thrombosis (SVT) is a manifestation of unusual site venous thromboembolism. Most common predisposing factors for SVT include liver cirrhosis, solid abdominal cancer, myeloproliferative neoplasms (MPN), and abdominal infection or inflammatory diseases. Complex balance between bleeding risk and the risk of thrombus extension or recurrence makes the management of SVT a clinical challenge. In this study, we reported clinical presentation and outcome data of patients with SVT followed in our center from January 2000 to December 2021, with a focus on MPN and cirrhotic patients.
Methods: We performed a retrospective review of clinical reports of 305 SVT patients. According to PLT count in patients with no active bleeding, anticoagulation treatment was started as soon as possible with: no treatment for a platelet count <30.000/μl; prophylactic dose of LMWH or related drugs for a platelet count range 30.000 -50.000/μl and therapeutic dose low-molecular-weight heparin (LMWH) followed by early initiation of vitamin-K antagonist (VKA; INR range 1.8-2.5) for a platelet count >50.000/μl. Moreover, cytoreductive therapy was administered in MPN patients and prophylaxis with beta-blockers and endoscopic therapies were applied in cirrhotic SVT. Cox regression analysis was used to identify independent predictors of recanalization and overall survival. The Kaplan-Meier method was performed to estimate the overall survival and the time to reach vessel recanalization.
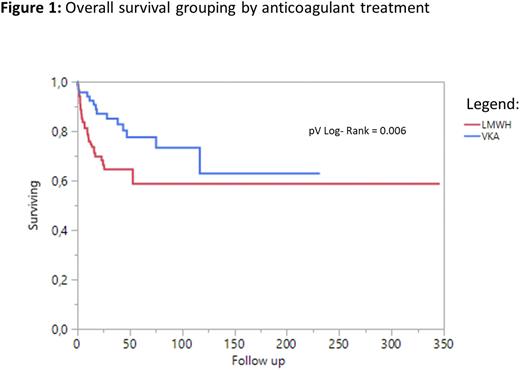
Results: In a median follow up of 16.1 months (range, 1-346), 305 patients experienced a SVT (median age 59 years; 68.2% males). Isolated portal vein thrombosis was the most common site of thrombosis (55.1%), followed by multiple venous involvement (28.9%). Six patients developed a Budd-Chiari syndrome. SVT were associated to chronic liver disease, solid cancer and abdominal infections in 212 (69.5%), 100 (32.8%) and 34 (11.5%) patients, respectively. Ninety-seven patients had splenomegaly. MPN was identified in 38 (12.5%) patients. Among these patients, JAK2 and CALR mutation were detected in 81.6% and 13.2%, respectively, and abnormal karyotype in 10.5%. Ascites and esophageal varices were present in 47.5% and 48.8% of patients, respectively. Therapeutic decisions were taken as a multidisciplinary team, involving the use of VKA and LMWH in 70 and 163 patients, respectively. In addition, trans-jugular intrahepatic portosystemic (TIPS) or other surgical shunting was undertaken in 12% and variceal banding in 11%. In a median duration therapy of 9.6 months, bleeding complications and recanalization were reported in 9.5% and 35.4% of patients, respectively. At univariate analysis, VKA exposure was associated with a significantly lower risk of bleeding events compared to LMWH (p=0.039), while esophageal varices (p=0.049), leukocytosis at time of thrombosis (p=0.048), liver cirrhosis (p=0.010) and solid tumor (p=0.021) were associated with lack of recanalization. Only one death was attributed to fatal bleeding, whereas 76 patients died for causes not related to anticoagulation (cirrhosis, cancer, MPN evolution) with a median OS was not reached (range, 107,89-NR). Factors associated with poor survival included age (p<0.001), MPN (p=0.047), recurrent thrombosis (p=0.041), alkaline phosphatase (p=0.013), gamma-GT (p<0.001), albumin (p=0.021), MELD score (p=0.004), lack of recanalization (p<0.001), bleeding event (p=0.043), ascites (p=0.009), and antithrombotic therapy (p=0.006, Figure 1). Among MPN patients, poor survival outcome was also associated with driver mutations (p=0.034), hemoglobin level at thrombosis (p<0.001), splenomegaly (p=0.019), and cytoreductive therapy (p=0.019).
Conclusions: Outcome in SVT patients mostly depends on the presence of an underlying MPN, liver failure, active bleeding, recurrence and recanalization rate. Moreover, the anticoagulant treatment was associated with a low bleeding incidence also in patients with major risk factors for bleeding (i.e. liver cirrhosis, cancer or esophageal varices).
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal